 (iStock/Getty Images)
(iStock/Getty Images)
Cognitive Impairment and Biomarkers in Venovenous ECMO
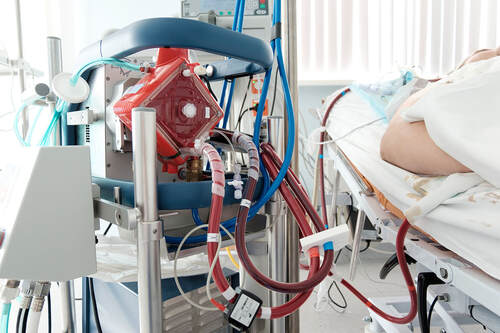
Patients who have severe lung disease and require venovenous extracorporeal membrane oxygenation (VV-ECMO) are at high risk for neurologic injuries (e.g. seizure, stroke, coma) due to hypoxia and anticoagulation during ECMO. They are also at risk for sustaining neurocognitive impairment due to prolonged stay in the intensive care unit. Early detection of these conditions will help clinicians effectively design preventative measures against neurologic injury. Our ECMO study is three-pronged. In order to identify evidence of any neurologic injury in VV ECMO patients, we are investigating whether blood samples of patients on VV ECMO contain microparticles and/or glial fibrillary acidic protein (GFAP), known biomarkers for traumatic brain injury. Elevated levels of GFAP are associated with poor neurological outcomes in pediatric ECMO survivors. However, no similar study has looked at GFAP and cognitive function in adult patients. Additionally, we are assessing patients’ comfort and awareness during mechanical ventilation while on ECMO. Lastly, we are evaluating patients’ cognitive function at hospital discharge, 30-day clinic follow-up at the University of Maryland Midtown campus, and 90-120 days post-hospital discharge (via telephone call).
Like our other prospective studies, members of the program conduct an initial screen of a potential ECMO patient. Patients must be getting VV ECMO and be > 18 years old to be eligible for enrollment. Patients are excluded if they are trauma patients requiring ECMO, require VA ECMO at any time prior to or doing enrollment, have abnormal neuroimaging studies prior to ECMO, have a history of seizure, dementia, Alzheimers’s, or Parkinson’s disease, or have any degree of traumatic brain injury.
Our group is collecting 9 blood samples for this study. Sample 1 is collected as a baseline once a patient is determined to require VV ECMO. Samples are subsequently collected at the first clinical blood draw after cannulation (Sample 2) and 2-5 days after cannulation (Samples 3-6). Sample 7 is drawn within 6 hours of decannulation, followed by Sample 8 at discharge and Sample 9 at the 30-day clinic follow-up. We monitor ECMO patients daily once they are enrolled and work with nurses to collect blood samples to be stored in our lab for future analysis.
Within 24 hours of patients coming off mechanical ventilation, our team interviews them using a questionnaire that asks them to rate their awareness and comfort levels during ECMO and intubation. At discharge, our team evaluates patients’ cognitive function using the Rivermead Questionnaire (RPQ), the modified Rankin Scale (mRS), and the Montreal Cognitive Assessment Version 1 (MoCA Version 1). At the 30-day clinic follow-up, patients complete the RPQ, mRS, and the Montreal Cognitive Assessment Version 2 (MoCA Version 2). At the 90--120 day follow up, our group assesses global outcomes using the Extended Glasgow Outcome Scale (GOSE).
We hope that this study will illuminate the cognitive outcomes of patients who are on VV ECMO. We aim to enroll 72 people to take part in this study. Half of our enrollees are control patients.
Patients who have severe lung disease and require venovenous extracorporeal membrane oxygenation (VV-ECMO) are at high risk for neurologic injuries (e.g. seizure, stroke, coma) due to hypoxia and anticoagulation during ECMO. They are also at risk for sustaining neurocognitive impairment due to prolonged stay in the intensive care unit. Early detection of these conditions will help clinicians effectively design preventative measures against neurologic injury. Our ECMO study is three-pronged. In order to identify evidence of any neurologic injury in VV ECMO patients, we are investigating whether blood samples of patients on VV ECMO contain microparticles and/or glial fibrillary acidic protein (GFAP), known biomarkers for traumatic brain injury. Elevated levels of GFAP are associated with poor neurological outcomes in pediatric ECMO survivors. However, no similar study has looked at GFAP and cognitive function in adult patients. Additionally, we are assessing patients’ comfort and awareness during mechanical ventilation while on ECMO. Lastly, we are evaluating patients’ cognitive function at hospital discharge, 30-day clinic follow-up at the University of Maryland Midtown campus, and 90-120 days post-hospital discharge (via telephone call).
Like our other prospective studies, members of the program conduct an initial screen of a potential ECMO patient. Patients must be getting VV ECMO and be > 18 years old to be eligible for enrollment. Patients are excluded if they are trauma patients requiring ECMO, require VA ECMO at any time prior to or doing enrollment, have abnormal neuroimaging studies prior to ECMO, have a history of seizure, dementia, Alzheimers’s, or Parkinson’s disease, or have any degree of traumatic brain injury.
Our group is collecting 9 blood samples for this study. Sample 1 is collected as a baseline once a patient is determined to require VV ECMO. Samples are subsequently collected at the first clinical blood draw after cannulation (Sample 2) and 2-5 days after cannulation (Samples 3-6). Sample 7 is drawn within 6 hours of decannulation, followed by Sample 8 at discharge and Sample 9 at the 30-day clinic follow-up. We monitor ECMO patients daily once they are enrolled and work with nurses to collect blood samples to be stored in our lab for future analysis.
Within 24 hours of patients coming off mechanical ventilation, our team interviews them using a questionnaire that asks them to rate their awareness and comfort levels during ECMO and intubation. At discharge, our team evaluates patients’ cognitive function using the Rivermead Questionnaire (RPQ), the modified Rankin Scale (mRS), and the Montreal Cognitive Assessment Version 1 (MoCA Version 1). At the 30-day clinic follow-up, patients complete the RPQ, mRS, and the Montreal Cognitive Assessment Version 2 (MoCA Version 2). At the 90--120 day follow up, our group assesses global outcomes using the Extended Glasgow Outcome Scale (GOSE).
We hope that this study will illuminate the cognitive outcomes of patients who are on VV ECMO. We aim to enroll 72 people to take part in this study. Half of our enrollees are control patients.